Dry Eye Treatment
Do you suffer from dry eye? Read more about it here or Contact us to book an appointment.

The Characteristics of Dry Eye Disease
Dry Eye Syndrome (DES) is a common disorder of tear film, which lubricate the eye and stop the surface from drying out. A chronic lack of sufficient lubrication and moisture on the surface of the eye leads to a range of symptoms varying from elusive but constant eye irritation to significant inflammation and even scarring on the cornea, and potentially some loss of vision. It can be related to either the quality or quantity of the tears.
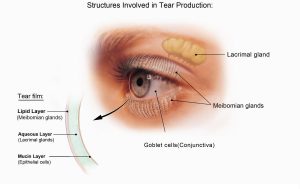
The characteristics of the tear film
The tear film is essential for eye health, comfort and good vision. With every blink of the eye, tears flow across the eye to keep it moist and wash away dust, debris and microorganisms that could damage the cornea and lead to an eye infection. Excess tears drain away through the tear ducts located in the upper and lower lids in the corner of the eye near the nose.
A normal tear film consists of three important components:
1. An outer, oily (lipid) component, produced by oil (Meibomian) glands in the eyelids that prevents tears from evaporating too quickly and helps tears remain on the eye.
2. A middle, watery (aqueous) component, contains the watery portion of tears as well as water-soluble proteins. This layer is produced by the main lacrimal gland and accessory lacrimal glands. It nourishes the cornea and the conjunctiva, the mucous membrane that covers the entire front of the eye and the inside of the eyelids.
3. An inner, mucous-like (mucin) component, produced by goblet cells in the conjunctiva (the clear membrane lining the eye). The mucins are an essential component that binds water from the aqueous layer to the ocular surface and therefore they ensure that the eye remains wet.
A problem with any of these tear film components can result in tear instability and dry eyes.
Causes of dry eye syndrome
Dry eye can affect anyone of any age and the Digital Revolution seems to have caused a new epidemic of DES across the developing world. Experts estimate that more than 100 million people worldwide suffer from dry eye of different severity.
A number of factors can increase a risk of dry eye syndrome. These include:
- Advancing age because we produce a smaller volume of tears
- Women have a higher prevalence of dry eye compared with men, especially menopausal and postmenopausal women
- Some ocular conditions including trachoma (sandy blight), chemical burns to the eyes, chronic eye lid inflammation, incomplete closure of the eyelids when blinking or sleeping
- Some medications such antihistamines, antidepressants, hormone replacement therapy, certain medication for high blood pressure, acne, and birth control pills can trigger dry eye.
- Some general health conditions including diabetes, rheumatoid arthritis, lupus, scleroderma, Sjogren’s syndrome, thyroid disorders, Parkinson’s disease and vitamin A deficiency can decrease tear production.
- Previous eye surgery such as cataract surgery and laser eye surgery (LASIK)
- Decreased blinking when working in front of a computer screen, reading, using a smartphone or other portable digital devices, or watching TV
- Long term contact lens wear as the lens absorption of the tear film by the lens, protein deposits on the lens and irritation of the conjunctiva by the lens
- Smoking can lead to increase tear evaporation
- Air-conditioned offices or supermarkets, rooms with ceiling fans and forced air heating systems because they decrease indoor humidity and/or hasten tear evaporation
- Arid climates and dry and windy climates
- Ocular irritants and allergens
Dry Eye Symptoms
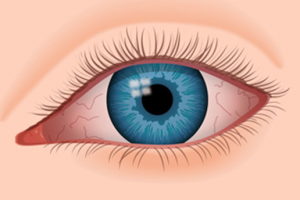
- Burning sensation
- Itchy eyes
- Sore eyes
- Heavy eyes
- Fatigued eyes
- Red eyes
- Dryness sensation
- Light sensitivity
- Blurred vision
- Excessive watering
- Foreign body sensation (the feeling that grit or some other object or material is ‘in” the eye)
Types of dry eye syndrome
There are two major forms of dry eye – aqueous deficient and evaporative. Both forms are related to deficiencies in the tear film.
- Evaporative dry eye
This form of dry eye is caused by an increase in tear evaporation due to abnormal tear film lipid layer. About 65-85% of all dry occurrences are caused by some form of evaporative dry eye, and it is believed that up to 86% of those have Meibomian gland dysfunction (MGD).
When the Meibomian glands do not produce enough lipids (meibum), the tear film breaks down very quickly, allowing the aqueous middle layer to evaporate, and patients typically feel a burning sensation, caused by exposure of the delicate corneal tissue to the atmosphere.
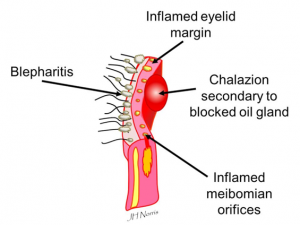
It is not yet clearly understood what causes MGD, but the progression of the condition typically starts with a thickening of the meibum and an increased keratinization of cells within the glands, leading to reduced lipids secretion and eventually blocked ducts. Once the glands reduce their lipids secretion patients begin to feel the irritation associated with dry eye. Further, decreased lipids secretion leads to inflammation of the eyelids, which further constricts the outlet ducts of the meibomian glands and increasingly restricts meibum secretion. Meibomian gland dysfunction is very often associated with blepharitis.
-
- Blepharitis
There are several forms of blepharitis – anterior and posterior.
Anterior blepharitis is generally associated with inflammation resulting from skin disorders caused by bacteria, parasites or allergic reactions, and is usually accompanied by flaking and scaling (sometimes called seborrheic blepharitis). This form can often be treated with lid hygiene and topical antibiotics.
Posterior blepharitis refers to inflammation resulting from meibomian gland dysfunction. Patients often have a mix of anterior and posterior blepharitis.

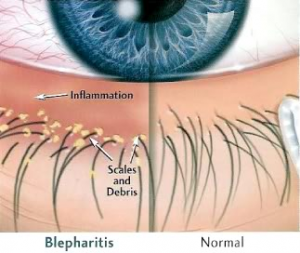
Blepharitis (which literally means inflammation of the eyelids) is a chronic condition, commonly associated with dry eye and dry skin. It causes mild, gritty sensations with sore eyelids. Occasionally it can be severe with changes in the eyelids resulting in lashes growing inwards. Blepharitis can be caused by bacterial and/or Demodex (a common mite) infection.
In some patients, bacteria commonly found on the skin, which normally are kept away from the surface of the eye and eyelids by a healthy tear film, proliferate along the lid margins. These bacteria release by-products, which have irritating effects on the eye, 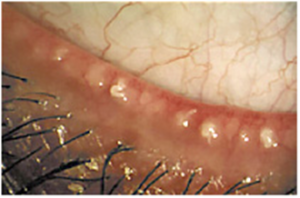 resulting in increased inflammation. This inflammation can lead to additional constriction of the meibomian glands, which further degrades the tear film causing more inflammation, and so on.
resulting in increased inflammation. This inflammation can lead to additional constriction of the meibomian glands, which further degrades the tear film causing more inflammation, and so on.
Another contributing factor in certain patients is a common mite (called Demodex), which triggers an overreaction of host immune and inflammatory responses. Demodex blepharitis is the most common but often overlooked external eye disease problem, causing ocular surface inflammation, changes in the oils produced by Meibomian glands, and prolonging and/or intensifying dry eye, rosacea and pterygium. Demodex is contracted and spread by either direct contact or dust containing eggs. 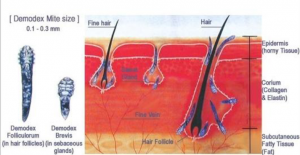
- Aqueous deficient dry eye

This form of dry eye is caused by a lack of aqueous tear secretion, which happens when the lacrimal glands produce the tears’ water component at a level that is too low, making it impossible for the surface of the eye to remain sufficiently hydrated. About 20% of all dry occurrences is caused by aqueous dry eye, which is most commonly diagnosed in women between 40 and 60 years of age.
Studies have found that chronic inflammation, combined with thickened tear ducts can cause tears to accumulate within the lacrimal gland, resulting in age-related aqueous tear deficiency dry eye. Other causes of lacrimal gland dysfunction include:
- Auto-immune disease
- Androgen deficiency
- certain medical conditions, such as diabetes, thyroid disorders and vitamin A deficiency
- Sjogren’s syndrome
Diagnosis of dry eye syndrome
The diagnosis can be made based on symptoms validated with the questionnaire (OSDI), a microscopic examination of the eyes, tear film and eye lids which will allow for diagnosis and grading of the condition.
The assessment also involves use of the Oculus Keratograph to examine and grade the Meibomian glands, tear film quantity and stability, and to track ocular surface redness.
If treatment is necessary, the Keratograph can compare the before and after treatment results to evaluate the success of the treatment.
Dry eye prevention and treatment
Dry eye syndrome is usually long-lasting condition which comes and goes with varying severity. Therefore, it is important to understand that ongoing treatment is required.
Lifestyle and home remedies
- Non-prescription eye drops (artificial tears)
They are a first line of treatment in dry eye syndrome and aim to lubricate the eyes and replace the missing moisture.
There are two major types of artificial tears:
-
- Aqueous supplementing eye drops such as Refresh, TheraTears, Biontears, Systane Ultra, HyloFresh and HyloForte. They provide lubrication and viscosity to the tears.
- Lipid-containing eye drops such as NovaTears or Systane Complete or Systane Balance and help to supplement abnormal lipid production, as they closely mimic the oil layer of the tear film.
Further, all eye drops come in two forms:
-
- Preservative that allow eye drops to be stored for up to three months after opening. However, they are known to cause adverse effects on the surface of the eye. Artificial tears with preservatives can be used up to four times a day.
- Non-preservative that should be recommended for patients with ocular allergies and those who need to use eye drops more than four times a day. They are individually packaged in small vials.
- Lubricating eye ointments
They coat the eyes, providing longer lasting relief from dry eyes, but these products are thicker and can cloud the vision. For this reason, ointments are best used before bedtime.
- Optimel, a Manuka honey-based eye drops or gel
Manuka honey has both antibacterial and anti-inflammatory properties. It is also believed that the hyperosmolarity of Optimel helps to draw oils out of the glands.
- Drops that reduce redness should be avoided as a solution for dry eye, as prolonged use can cause more irritation
- While reading, watching television or working on the computer remember to blink frequently.
- Lower the level of your computer monitor so your eyes are looking downwards while you work – this will slow down evaporation of your tears.
- Take frequent breaks to rest your eyes.
- Drink 8 to 10 glasses of water per day to keep your body well hydrated.
- Use a humidifier at home and/or at work — especially where there is air-conditioning. Water loving plants with big leaves can also release water to atmosphere and increase humidity in a work area
- Wear wrap-around spectacles when you are outside to stop the wind drying your eyes.
- Stop smoking and avoid environments that contribute to dryness such as an overly warm room or smoky atmosphere.
- Avoid air blowing in your eyes. Don’t direct hair dryers, car heaters, air conditioners or fans toward your eyes.
- Apply artificial tear drops as required.
With the awareness that blepharitis is the primary causative factor in the majority of dry eye patients a regular routine of eye hygiene and Meibomian gland expression is essential to relieve the symptoms. It may take several weeks before there is an improvement and it should be continued for a long time or the discomfort can return.
Steps to treat blepharitis
- At home
- Warm compress (e.g. an eye mask warmed up in the microwave for 10-20 sec) applied to the eyelids for 10 min.
- Fingertip or cotton bud gentle massage to express the oil from the tiny glands in the eyelids. Alternatively oils can be expressed by pinching a portion of the lid margin with the thumb and forefinger.
- Cleaning the base of the lids and lashes using Blephadex wipes or Opti-Soothe wipes. Begin on the nasal side and move across the lid to the temporal side. The edges of the eyelids should be gently scrubbed to remove all the oil and build up secretions.
- In office
 Blephex gently exfoliates the eyelids and eyelashes removing the exotoxin –laden biofilm that accumulates on the eyelid, providing rapid relief from eyelid inflammation symptoms. This painless procedure effectively removes the scurf and bacterial debris that build up along the lid margin. This debris is responsible for most of the low-grade inflammatory blepharitis, the primary cause of the chronic dry eye disease.
Blephex gently exfoliates the eyelids and eyelashes removing the exotoxin –laden biofilm that accumulates on the eyelid, providing rapid relief from eyelid inflammation symptoms. This painless procedure effectively removes the scurf and bacterial debris that build up along the lid margin. This debris is responsible for most of the low-grade inflammatory blepharitis, the primary cause of the chronic dry eye disease.

- Blephasteam followed by expression of clogged Meibomian glands. Using heat and moisture through thermal goggles for just 10 minutes, the goggles warm the oil in the lids to the temperature needed to liquefy and unblock glands. Following this relaxing time, the Optometrist manually expresses the glands to unblock them fully.
Prescription medications
- Topical drugs to reduce eyelid inflammation
Inflammation along the edge of the eyelids can keep oil glands from secreting oils into the eyes and contributes to both signs and symptoms of the disease. Ointment such as Azithromycin 1% attacks certain bacteria yet also have anti-inflammatory properties and have been shown to improve meibum quality. The ointment should be applied to the eye itself or to the lid margin using clean fingers or a cotton bud at bedtime.
- Eye drops to control ocular surface inflammation
- Steroid eye drops
They are well known as potent treatments of inflammation, and short-term, high frequency doses are effective in managing exacerbations of dry eye, improving symptoms and signs. While effective in the short-term, steroid eye drops have limited use in chronic management due to associated risk of serious complications, including infections, increased ocular pressure and cataract formation. Treatment options include FML, Flarex, Flucon, Maxidex and Prednisolone Forte.
-
- Anti-inflammatory eye drops
Cyclosporine 0.05% eye drops has been recommended for chronic management of dry eyes as it doesn’t cause the side-effects associated with steroid eye drops. It stimulates tear production and has an anti-inflammatory effect.
Other procedures
- Punctal plugs
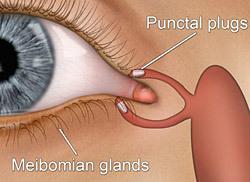
They are recommended for patients with persistent and more serious eye irritation due to dry eye syndrome. This treatment is recommended for preventing the tears leaving the eyes too quickly.
Tear ducts can be plugged with tiny silicon plugs, which are a removable first line of treatment in dry eye syndrome. Punctal plugs aim to lubricate the eyes and replace the missing moisture. Tear ducts can also be permanently plugged with a procedure that uses heat (thermal heating).
- Special contact lenses (bandage lenses or scleral lenses)
They alleviate dry eye symptoms and optimize visual function as they trap moisture between the lens and ocular surface.
Supplementary treatment
- Flaxseed oil or fish oil
Daily supplements of flaxseed oil or fish oil, when used alone or together with lubricating eye drops, appear to reduce dry eye symptoms, including burning, stinging, redness and intermittent visual disturbances. Both oils are excellent sources of omega-3 fatty acids.
Flaxseed oil contains high levels of omega-3 (ALA) that is converted during digestion into two different omega-3 fatty acids (called EPA and DHA). EPA and DHA are found in fish oil.
Fish oil benefits can be obtained by eating grilled cold-water fish at least three times a week. Good sources of EPA and DHA omega-3s are salmon, sablefish, tuna and halibut. The dose is about 1 gram (1000mg) of EPA and DHA omega-3 fatty acids daily. For instance, to get the recommended 1 gram of omega-3 fatty acids, the patient would need to eat one to two servings of salmon, four to seven servings of cod, or four servings of prawns per day. Therefore, a fish oil supplement should be considered to get the recommended 1 gram of omega-3 fatty acids per day.
Do you suffer from dry eye? Contact us today to book an appointment.
